Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression Prior Authorization Form Fax to 1 877 243 6930 Phone 1 800 285 9426 Part D Prior Authorization Form Medicare Part D Fax to 1 800 693 6703 PDF 4 7 Stars 26 Ratings 1 771 Downloads
You can sign up to use the electronic prior authorization ePA system through CoverMyMeds all that is needed is a computer and an internet connection How to get started Visit CoverMyMeds to see if it s already integrated with your pharmacy system and start saving time today You must complete this form to authorize Prime Therapeutics information about you with someone else to share Note Under the law an authorization for use or disclosure of psychotherapy notes cannot be combined with an authorization for other health care information Fill in the member s name ID number and date of birth
Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression

Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression
https://i2.wp.com/eforms.com/images/2017/05/Prime-Therapeutics-Prior-Authorization-Form.png?fit=2550%2C3301&ssl=1

Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression Printable Forms
https://www.sample-templatess123.com/wp-content/uploads/2016/03/Prime-Therapeutics-Prior-Authorization-Form-Example.jpg

Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression Printable Forms
https://www.sample-templatess123.com/wp-content/uploads/2016/03/Example-Of-Prime-Therapeutics-Prior-Authorization-Form.jpg
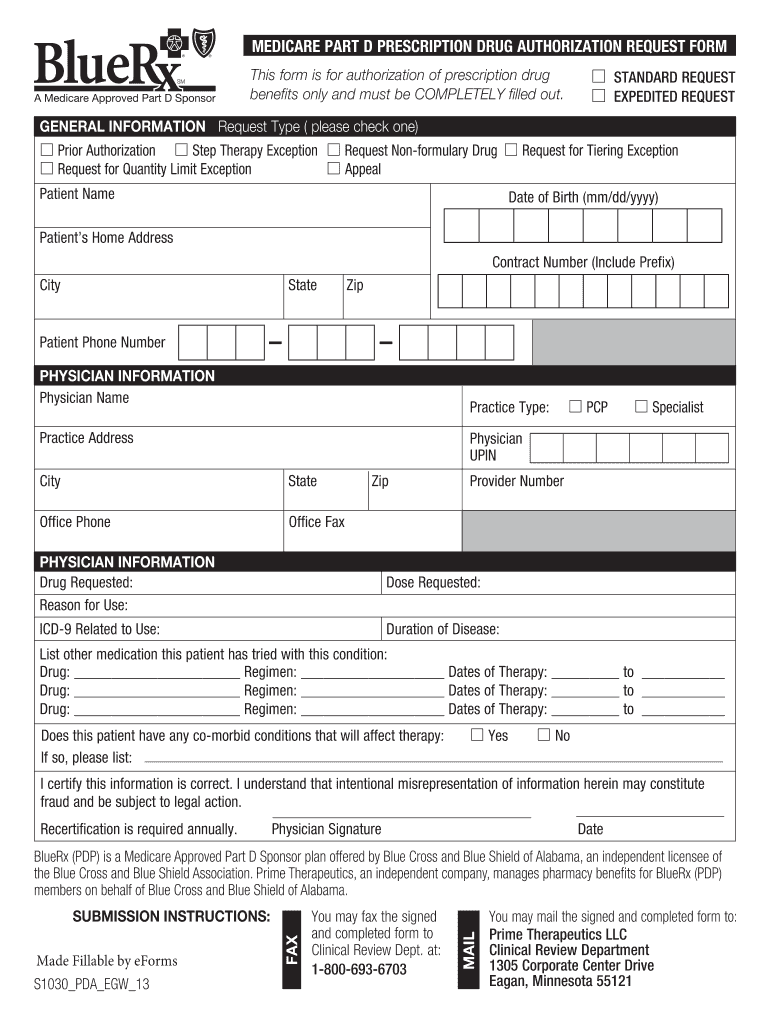
PROPROTEIN CONVERTASE SUBTILISIN KEXIN TYPE 9 PCSK9 INHIBITORS PRIOR AUTHORIZATION REQUEST PRESCRIBER FAX FORM Only the prescriber may complete this form This form is for prospective concurrent and retrospective reviews The following documentation is REQUIRED Incomplete forms will be returned for additional information Please fax or mail this form to Blue Cross and Blue Shield of Illinois c o Prime Therapeutics LLC Clinical Review Department 1305 Corporate Center Drive Eagan Minnesota 55121 TOLL FREE Fax 877 243 6930 Phone 800 285 9426 CONFIDENTIALITY NOTICE This communication is intended only for the use
PRIOR AUTHORIZATION REQUEST PRESCRIBER FAX FORM Only the prescriber may complete this form This form is for prospective concurrent and retrospective reviews Incomplete forms will be returned for additional information The following documentation is required for preauthorization consideration The Prime Therapeutics Provider Manual is a comprehensive guide for health care providers who work with Prime a pharmacy benefit management company The manual covers topics such as Prime s contact information claims processing prior authorization drug utilization management and more The manual is updated periodically to reflect the latest policies and procedures Download the PDF
More picture related to Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression

Prime Therapeutics Prior Authorization Form Fill Out Sign Online DocHub
https://www.pdffiller.com/preview/26/660/26660096/large.png

Prime Therapeutics Prior Authorization Form To Download Sample Templates Sample Templates
https://www.sample-templatess123.com/wp-content/uploads/2016/03/Prime-Therapeutics-Prior-Authorization-Form-To-Download.jpg

Tyrese s Depression Medication Rexulti 5 Things You Need To Know Right Now
https://www.sohh.com/wp-content/uploads/2017/11/Rexulti.jpg
Start saving time today by filling out this prior authorization form electronically Visit www NaviNet hzdpa to register and then begin using this free service as part of your existing NaviNet account PATIENT AND INSURANCE INFORMATION Today s Date PRESCRIBER CLINIC INFORMATION Prior Authorization Required on some medications before your drug will be covered If your health plan s formulary guide indicates that you need a Prior Authorization for a specific drug your physician must submit a prior authorization request form to the health plan for approval
Your doctor will need to submit a prior authorization request to Prime Therapeutics which must be approved before you can continue to receive coverage for these drugs The Prior Authorization form that your physician will need to complete to request an approval can be found on the MyPrime website Quantity Limit Consideration A new version of Prime s Provider Manual with an efective date of Apr 15 2021 is available for review on Prime s website at www PrimeTherapeutics Resources Pharmacy provider Provider manual Please continue to use the October 2020 Provider Manual until Apr 15 2021
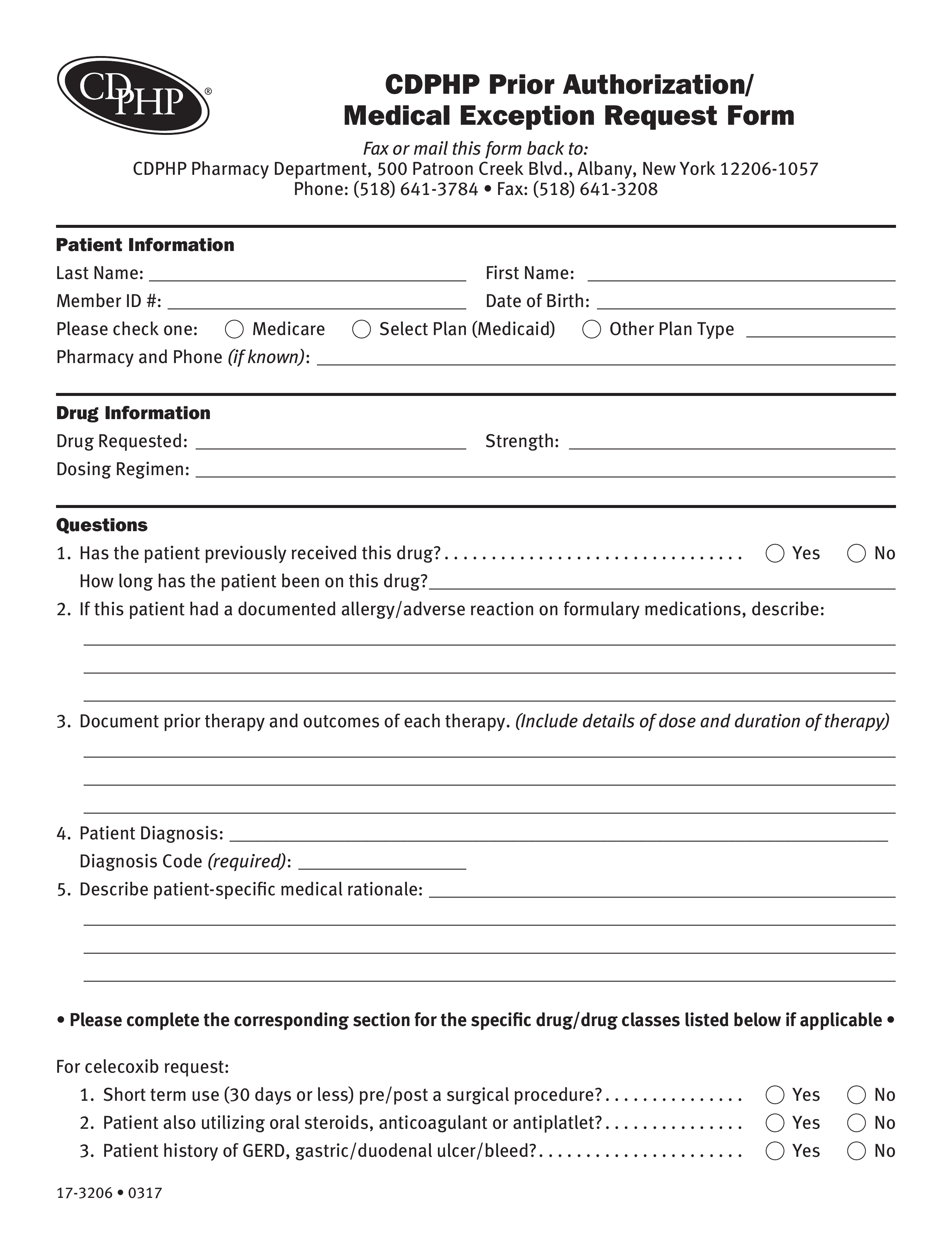
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms Bank2home
https://eforms.com/images/2017/05/CDPHP-Prior-Authorization-Form.png
Prime Therapeutics Prior Authorization Form Pdf Amulette
http://amulettejewelry.com/wp-content/uploads/2018/09/prime-therapeutics-prior-authorization-form-pdf-global-prior-authorization-form-791x1024-768x994.jpg

https://eforms.com/prior-authorization/prime-therapeutics/
Prior Authorization Form Fax to 1 877 243 6930 Phone 1 800 285 9426 Part D Prior Authorization Form Medicare Part D Fax to 1 800 693 6703 PDF 4 7 Stars 26 Ratings 1 771 Downloads

https://www.primetherapeutics.com/resources/electronic-prior-authorization/
You can sign up to use the electronic prior authorization ePA system through CoverMyMeds all that is needed is a computer and an internet connection How to get started Visit CoverMyMeds to see if it s already integrated with your pharmacy system and start saving time today
Rexulti Dosage Drug Information MIMS Hong Kong
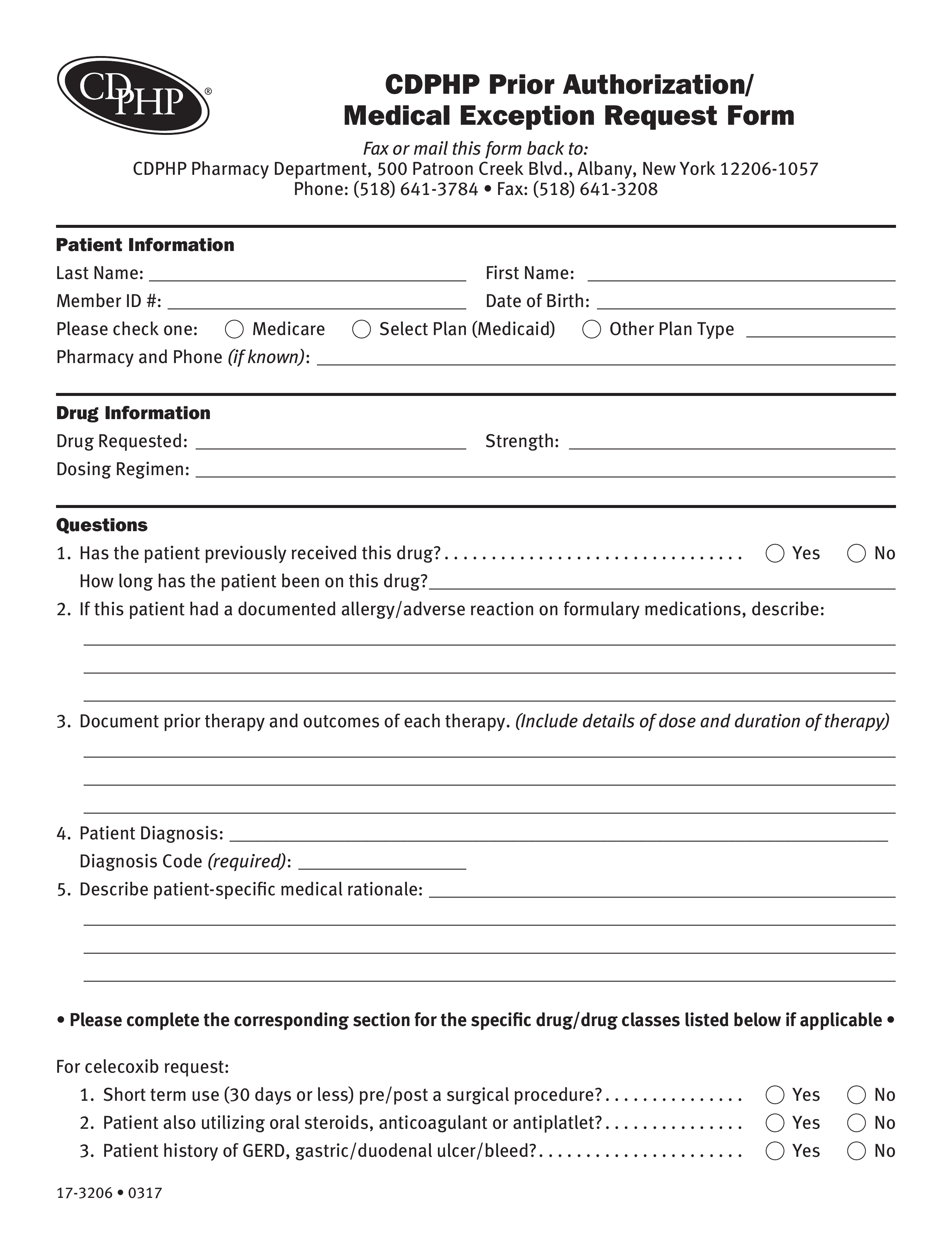
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms Bank2home

Rexulti Prices Coupons Savings Tips GoodRx

FDA Approves Rexulti For Agitation Associated With Dementia Due To Alzheimer s
Prime Therapeutics Part D Prior Authorization Form Part D Drug Authorization Request Form Fill

Prime Therapeutics Pharmacy Prior Authorization Form PharmacyWalls

Prime Therapeutics Pharmacy Prior Authorization Form PharmacyWalls

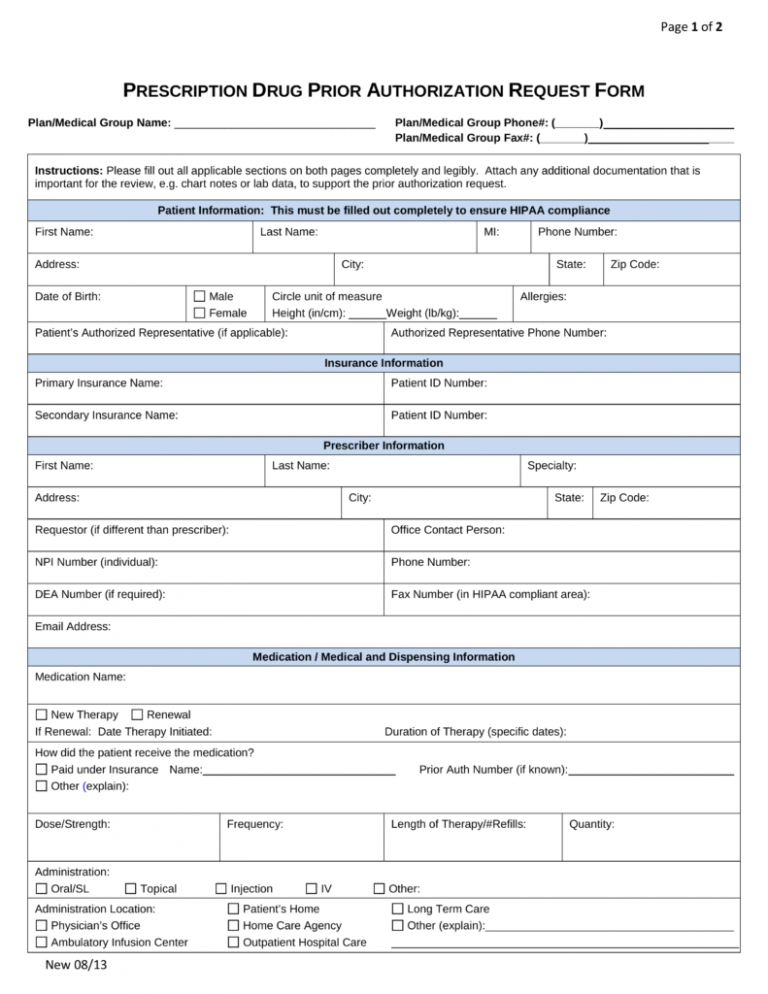
Fillable Prescription Drug Prior Authorization Request Form Printable PlanForms

Servicios Farmac uticos Especializados Tienda Para Pacientes

Rx Item Rexulti Brexpiprazole 0 25Mg Tab 30 By Otsuka America
Prime Therapeutics Printable Prior Authorization Form Rexulti Major Depression - PRIOR AUTHORIZATION REQUEST PRESCRIBER FAX FORM Only the prescriber may complete this form This form is for prospective concurrent and retrospective reviews Incomplete forms will be returned for additional information The following documentation is required for preauthorization consideration