Cigna Botox Prior Authorization Form Printable Prior Authorization How to request precertifications and prior authorizations for patients Depending on a patient s plan you may be required to request a prior authorization or precertification for any number of prescriptions or services A full list of CPT codes are available on the CignaforHCP portal For Medical Services Description of service
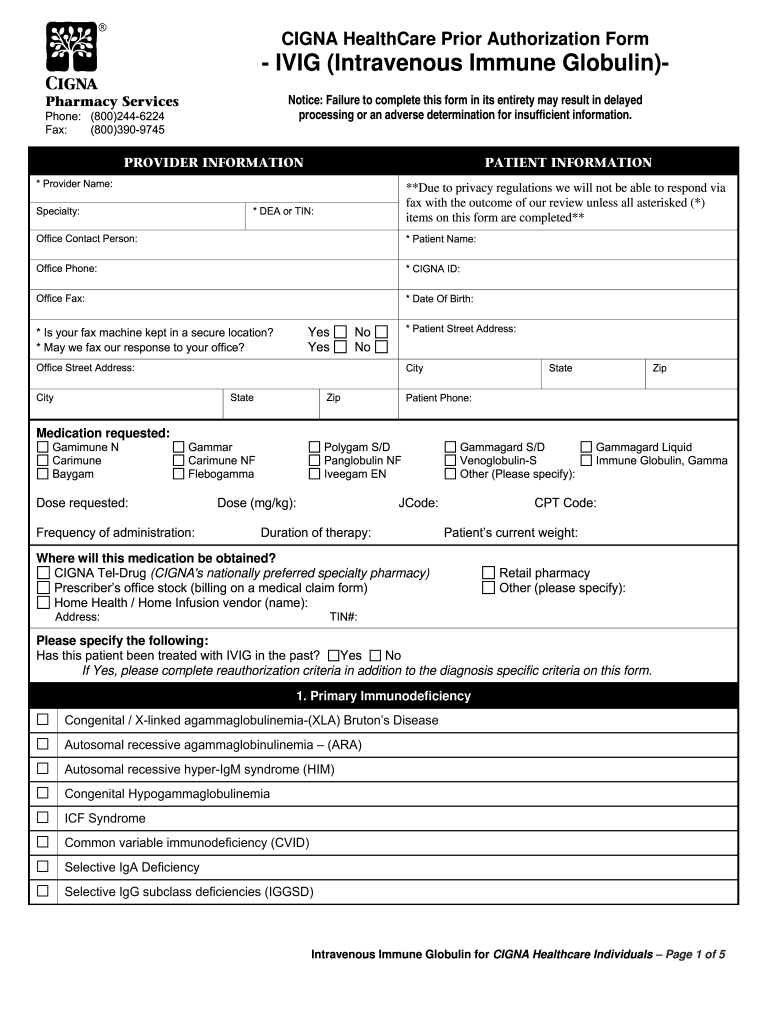
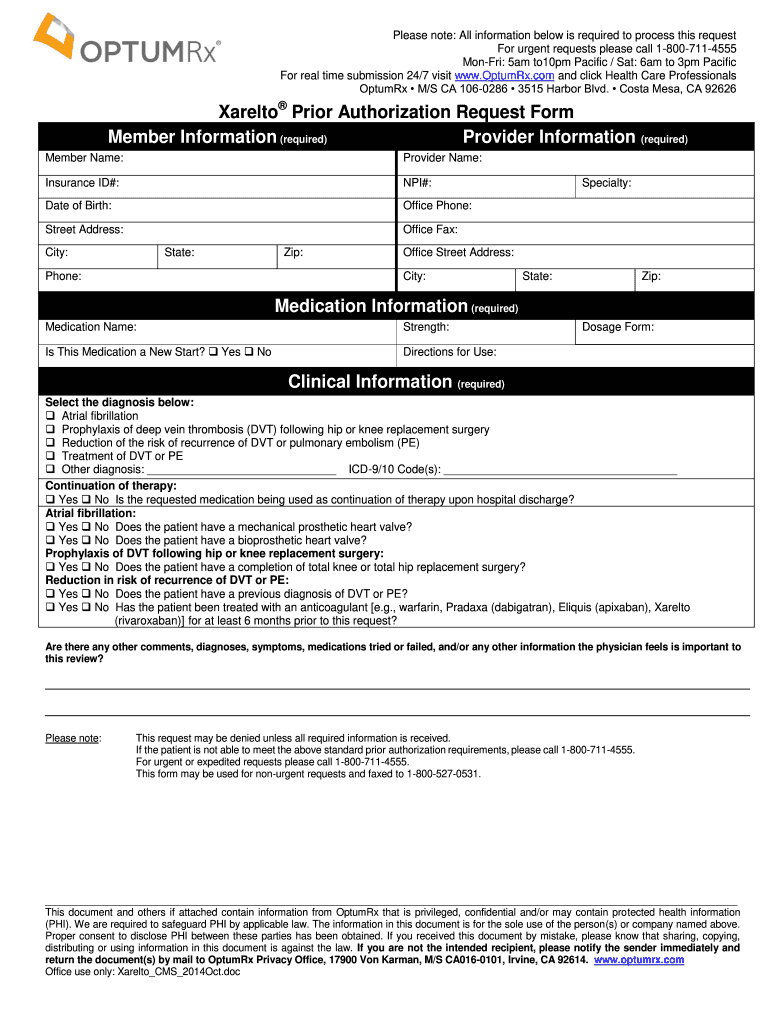
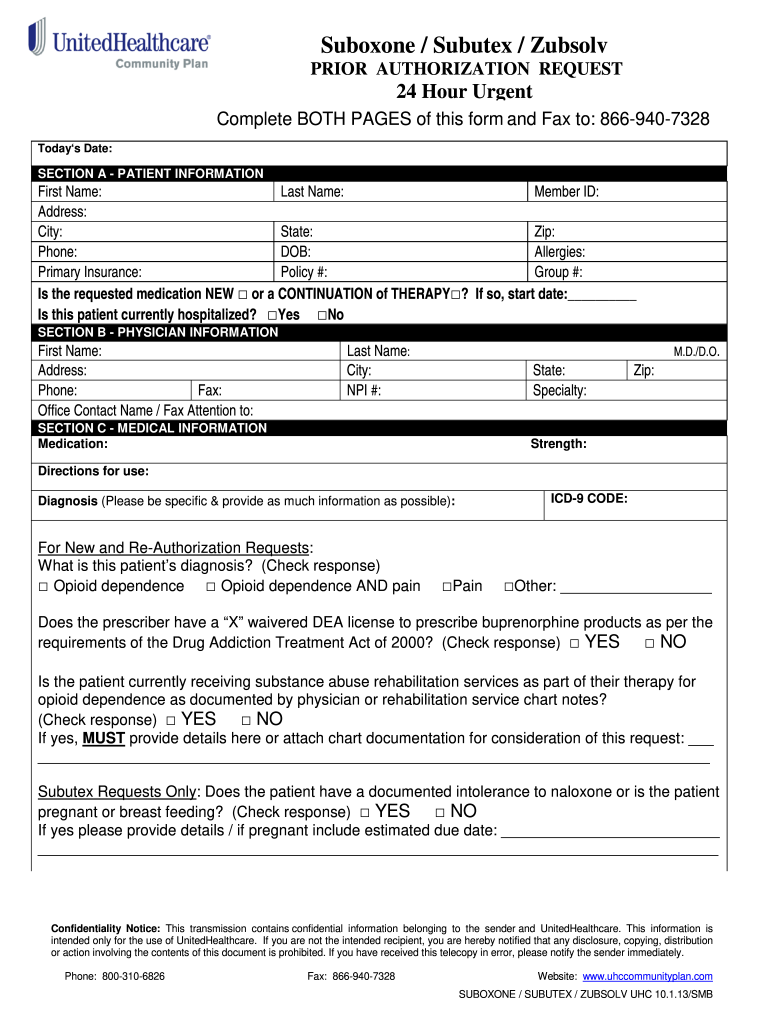
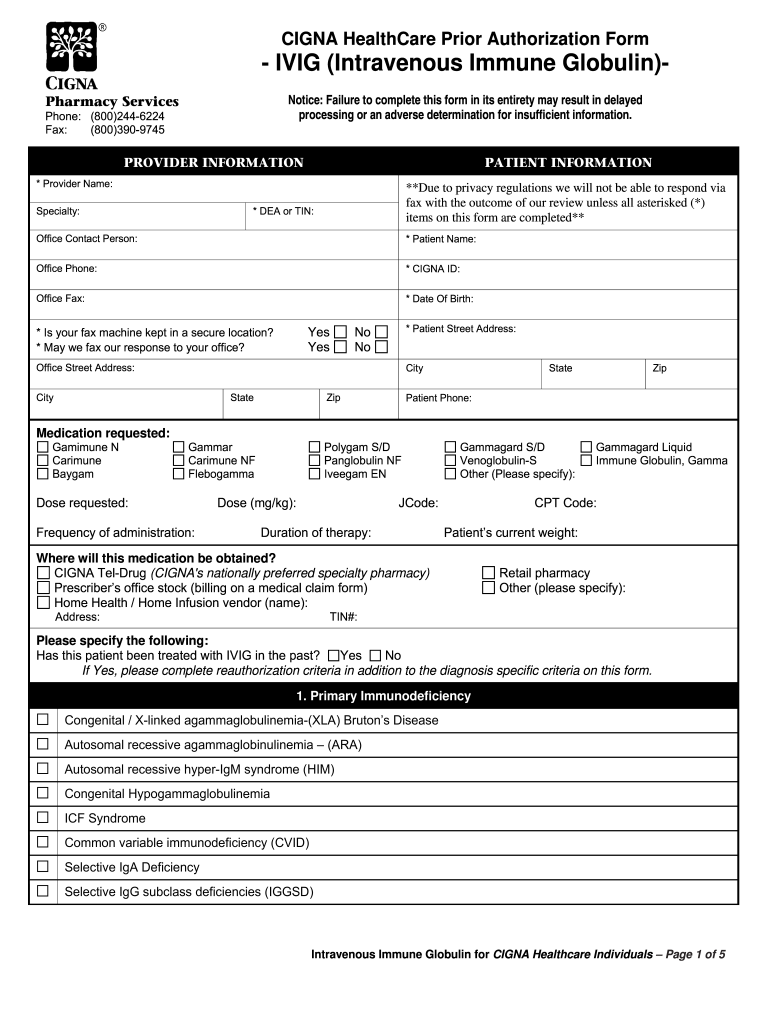
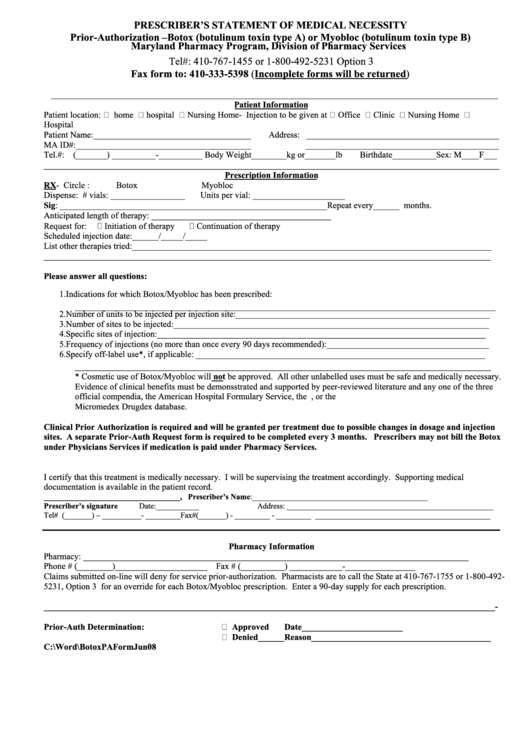
General Drug Prior Authorization Forms The prescription forms center contains tools that may be necessary for filing certain claims appealing claims changing information about your office or receiving authorization for certain prescriptions CIGNA HealthCare Prior Authorization Form Botox botulinum toxin type A Notice Failure to complete this form in its entirety or include chart notes may result in delayed processing or an adverse determination for insufficient information Spasticity due to cerebral palsy including spastic equinus foot deformities
Cigna Botox Prior Authorization Form Printable
Cigna Botox Prior Authorization Form Printable
https://www.pdffiller.com/preview/0/151/151879/large.png
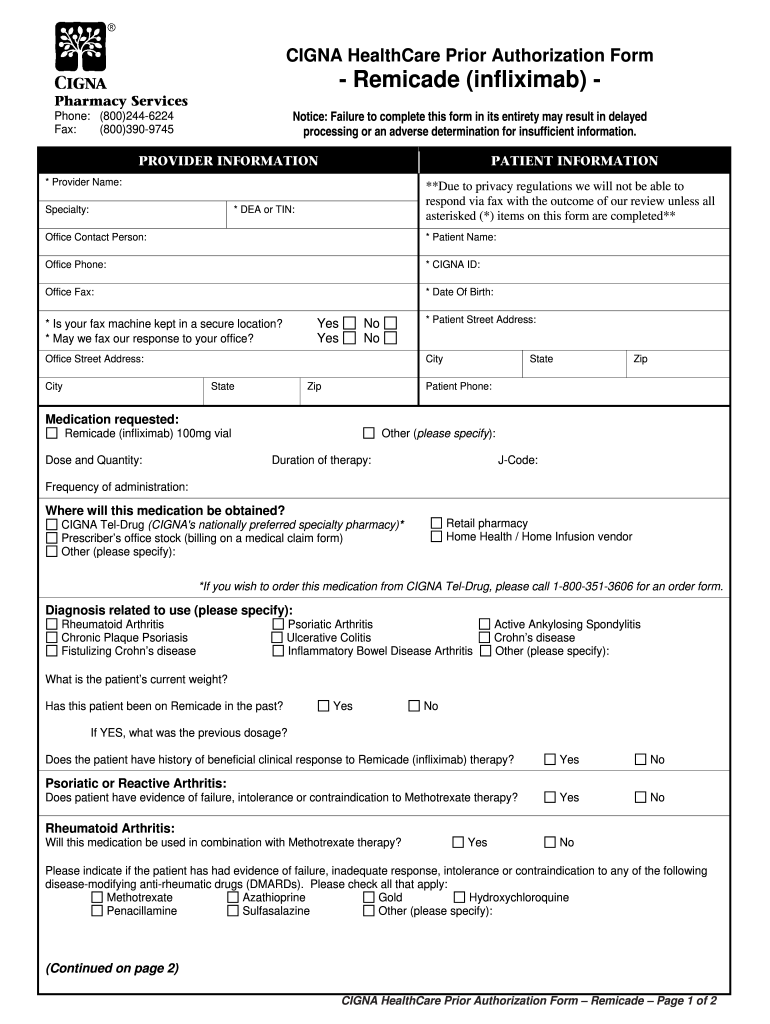
Cigna Prior Authorization Form For Remicade Infusion 2020 Fill And Sign Printable Template
https://www.pdffiller.com/preview/0/151/151994/large.png
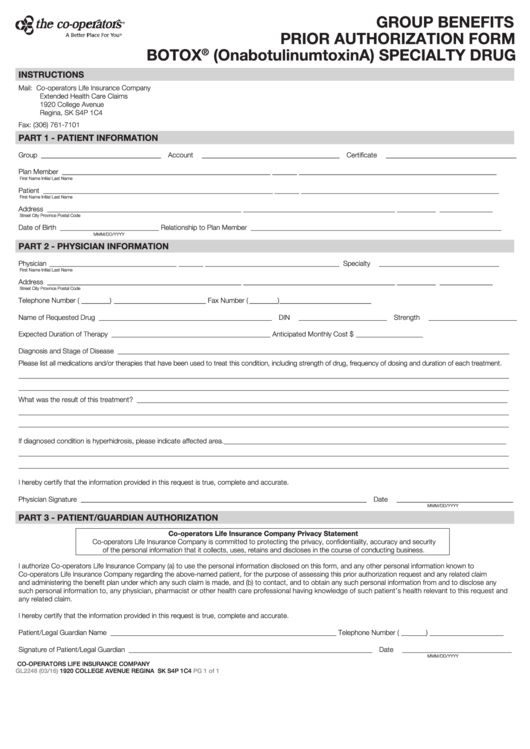
Fillable Form Gl2248 Group Benefits Prior Authorization Botox Onabotulinumtoxina Specialty
https://data.formsbank.com/pdf_docs_html/183/1831/183179/page_1_thumb_big.png
Knowledge Center Wellness Library Botulinum Toxin Botox Botulinum Toxin Botox The injection of botulinum toxin commonly known as Botox has become very popular for reducing wrinkles and rejuvenating the aging face Save Time Submit Online at www covermymeds main prior authorization forms cigna or via SureScripts in your EHR Our standard response time for prescription drug coverage requests is 5 business days If your request is urgent it is important that you call us to expedite the request
PRIOR AUTHORIZATION REQUEST FORM FOR HEALTH CARE SERVICES FOR USE IN INDIANA encourages insurers Form for administrators for use in Indiana and others Intended authorization use completed by An to the issuer may also prior authorization 1 to request an on to its website of a health an eligibility Botox Dysport Xeomin sustained closure of the eyelids caused by involuntary contractions of BOTH of the following Treatment for blepharospasm characterized by intermittent or the orbicularis oculi muscle Page 2 of 30 Coverage Policy Number 1106 Condition Product Criteria for Use
More picture related to Cigna Botox Prior Authorization Form Printable
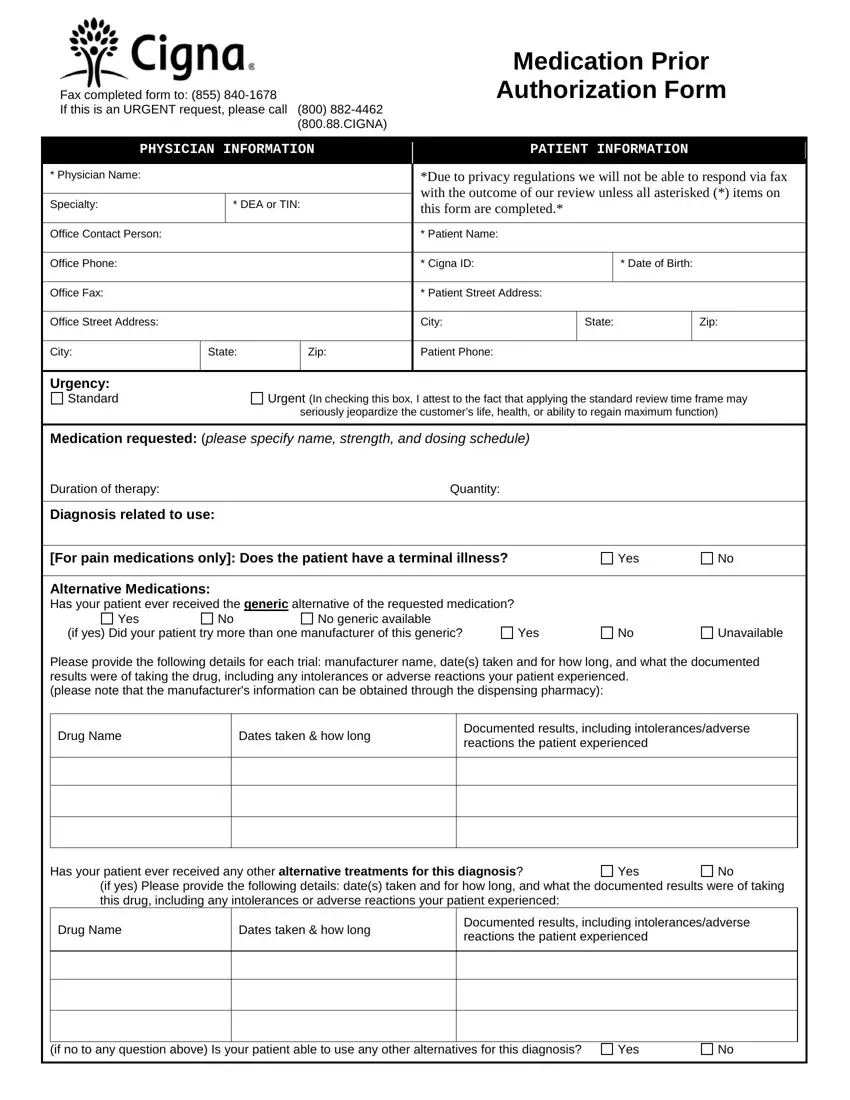
Cigna Prior Auth Form Fill Out Printable PDF Forms Online
https://formspal.com/pdf-forms/other/cigna-prior-auth-form/cigna-prior-auth-form-preview.webp

Botox Treatment Form Pdf Consent Form
https://consent-forms.com/wp-content/uploads/2023/01/free-botox-botulinum-toxin-patient-consent-forms-pdf-2.jpg
Optumrx Prior Auth Form 2020 2021 Fill And Sign Free Download Nude Photo Gallery
https://www.pdffiller.com/preview/41/851/41851770/large.png
Medical Forms Request a Medical ID card Change Primary Care Physician Medical Appeal Request English PDF Spanish PDF Chinese PDF Medical Claim Form English PDF Spanish PDF Direct Member Reimbursement DMR English PDF Botox CCRD Prior Authorization Form PDF Prior Authorization Form for Botox Botulinum Therapy 1106 PDF Cigna Coverage Policy 1106 Calcitonin Gene Related Peptide CGRP Inhibitors for Employer Group Plans PDF Cigna Coverage Policy IP0050 CGRP Inhibitors CCRD Prior Authorization Form PDF Prior Authorization Form for CGRP Inhibitors
01 Edit your cigna botox prior authorization form online Type text add images blackout confidential details add comments highlights and more 02 Sign it in a few clicks Draw your signature type it upload its image or use your mobile device as a signature pad 03 Share your form with others Send cigna botox form via email link or fax CGRP Inhibitors CCRD Prior Authorization Form Fax completed form to 855 840 1678 If this is an URGENT request please call 800 882 4462 800 88 CIGNA CGRP Inhibitors Aimovig Ajovy Emgality While taking the requested drug will you patient also receive Botox during the same time Yes No
Prior Authorization Request Form Fill Online Printable Fillable Blank PdfFiller
https://www.pdffiller.com/preview/37/293/37293717/large.png

Cigna Botox Prior Authorization Form Fill Online Printable Fillable Blank PdfFiller
https://www.pdffiller.com/preview/0/151/151904/large.png
https://www.cigna.com/health-care-providers/coverage-and-claims/prior-authorization
Prior Authorization How to request precertifications and prior authorizations for patients Depending on a patient s plan you may be required to request a prior authorization or precertification for any number of prescriptions or services A full list of CPT codes are available on the CignaforHCP portal For Medical Services Description of service

https://static.cigna.com/assets/chcp/resourceLibrary/forms/formsPrescriptionPriorAuthFormsListing.html
General Drug Prior Authorization Forms The prescription forms center contains tools that may be necessary for filing certain claims appealing claims changing information about your office or receiving authorization for certain prescriptions
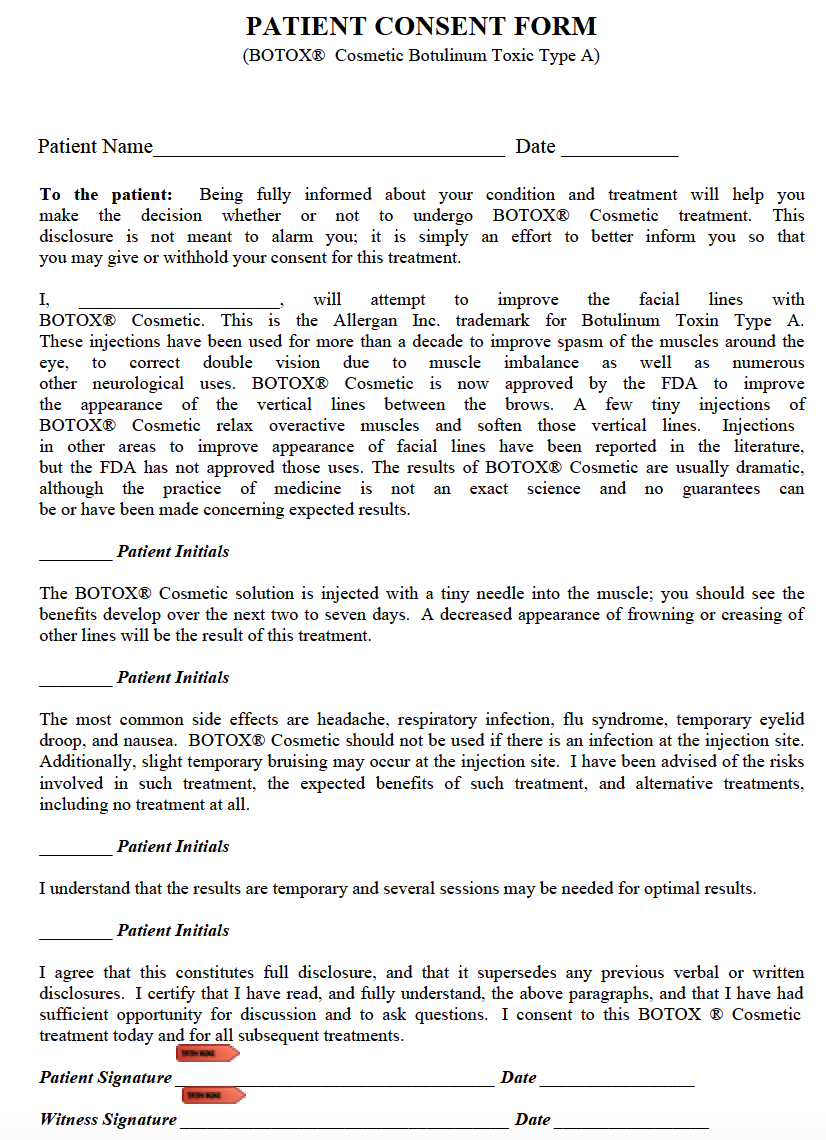
Printable Botox Consent Form Printable Form Templates And Letter
Prior Authorization Request Form Fill Online Printable Fillable Blank PdfFiller
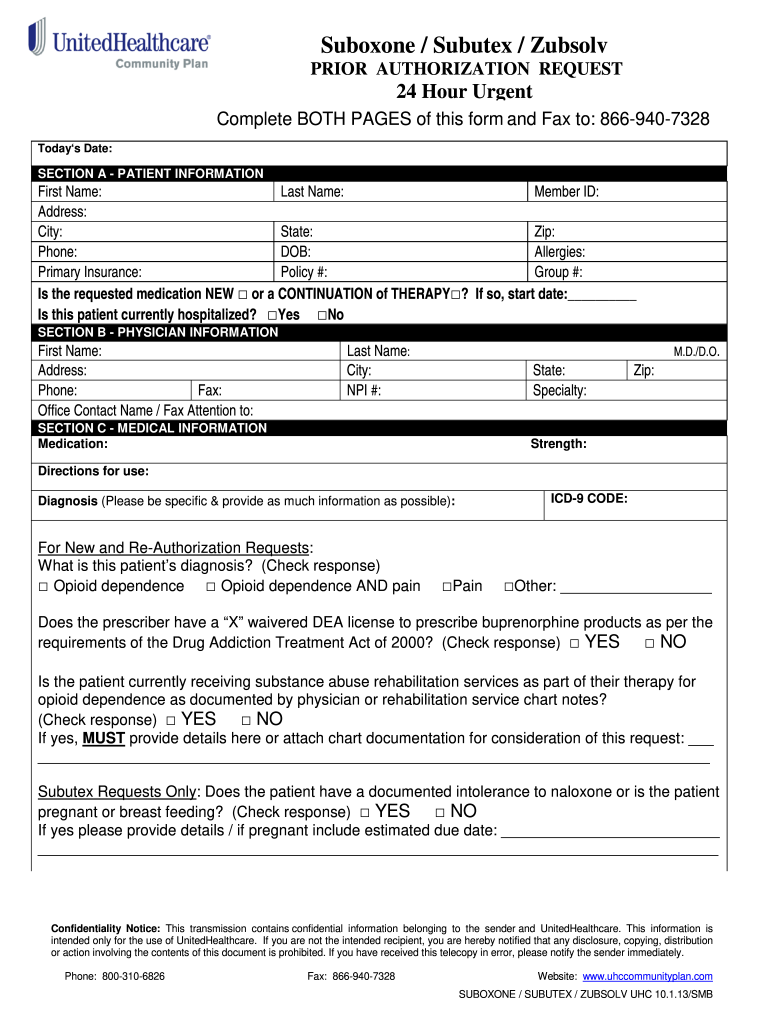
Botox Or Myobioc Prior Authorization Form Prescriber S Statement Of Medical Necessity
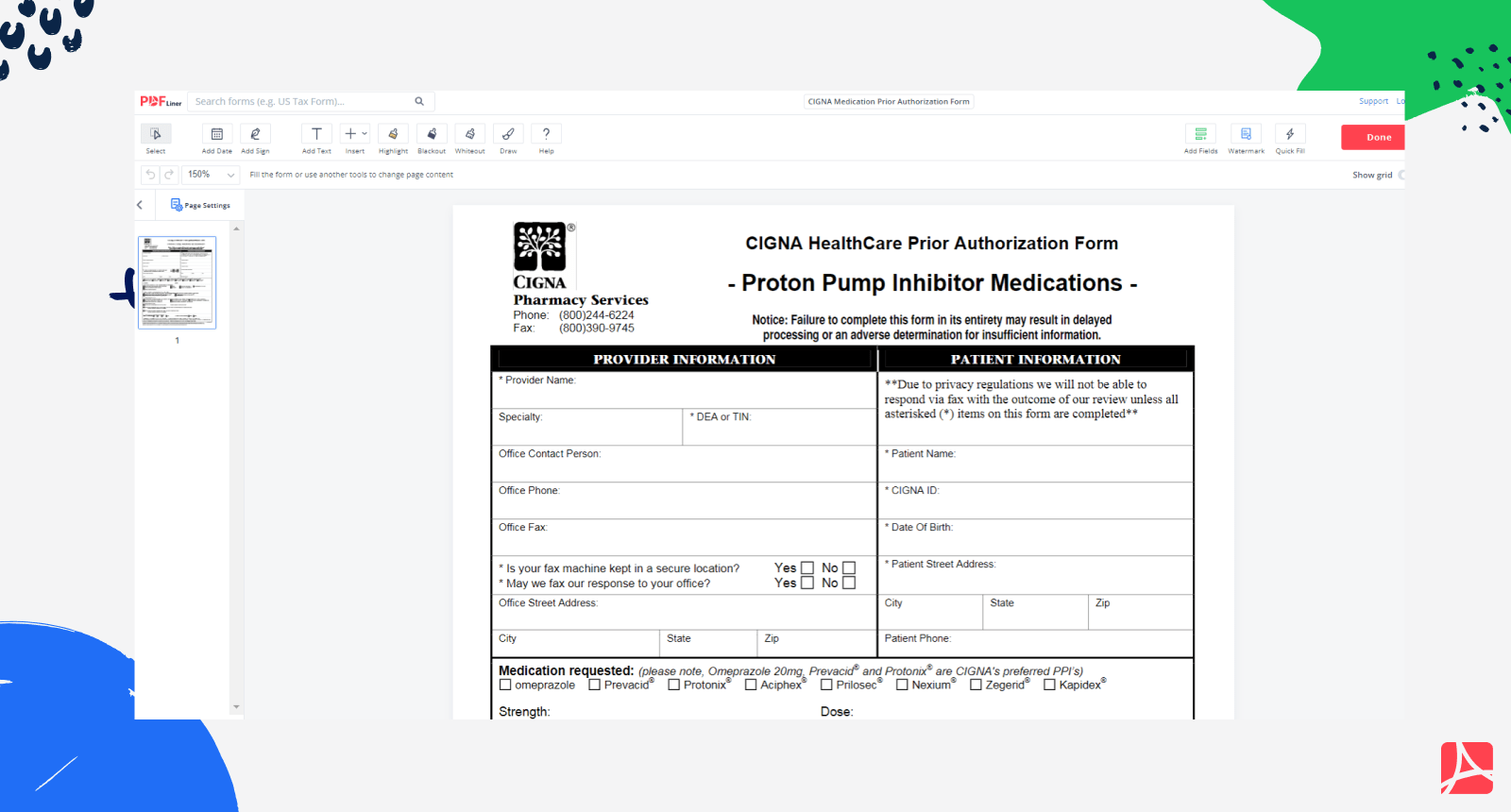
CIGNA Medication Prior Authorization Form PDF Blank PDFliner

Covermymeds Humana Prior Auth Form 3 Metzger Snate1989

Fillable Prescription Drug Prior Authorization Request Form Printable PlanForms

Fillable Prescription Drug Prior Authorization Request Form Printable PlanForms

Cigna Botox Prior Authorization Form Printable Printable Forms Free Online

Fillable Online Static cignaassetschcpBotox CCRD Prior Authorization Form Cigna Fax Email

Cigna Healthcare Prior Authorization Form 2010 2022 Fill And Sign Printable Template Online
Cigna Botox Prior Authorization Form Printable - Botox Dysport Xeomin sustained closure of the eyelids caused by involuntary contractions of BOTH of the following Treatment for blepharospasm characterized by intermittent or the orbicularis oculi muscle Page 2 of 30 Coverage Policy Number 1106 Condition Product Criteria for Use