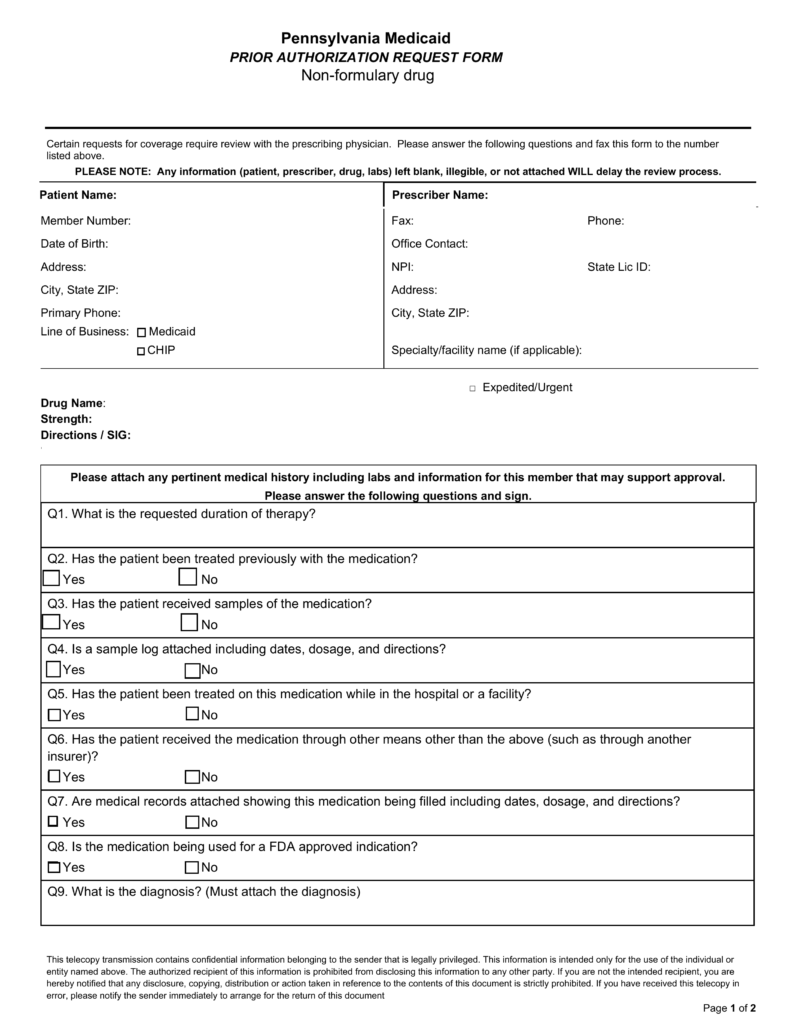
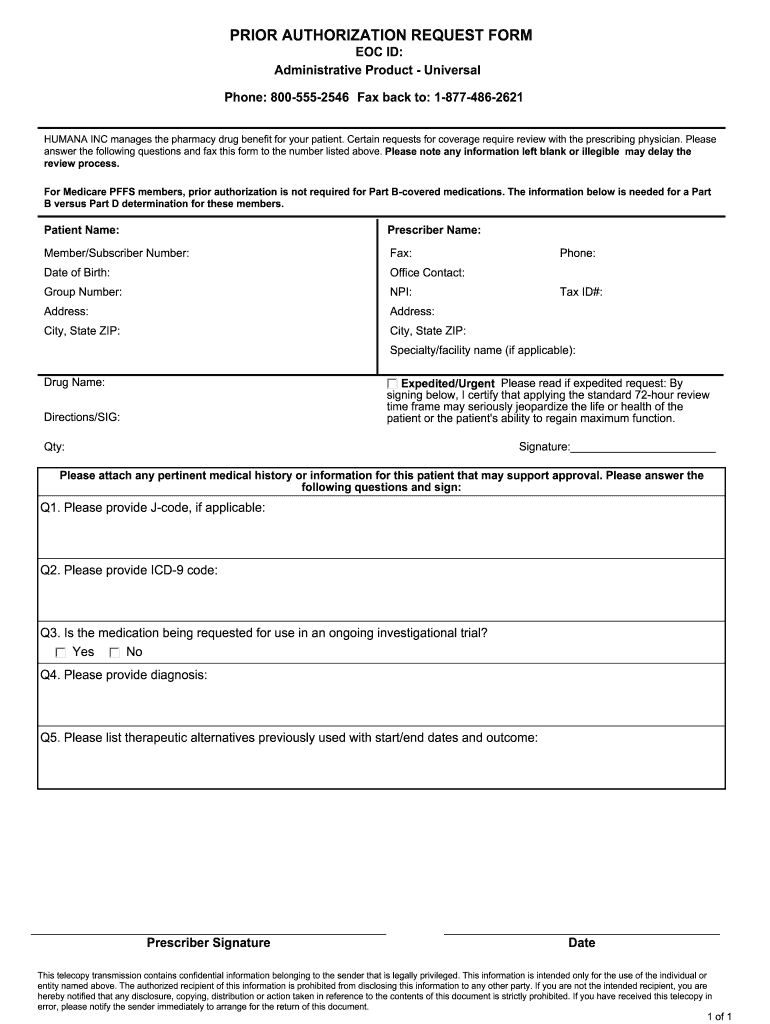
Printable Humana Prior Authorization Form Authorization Referral Request Form Please complete all fields on this form and be sure to include an area code along with your telephone and fax numbers To verify benefits call commercial 800 448 6262 Medicare 800 457 4708 Florida Medicaid 800 477 6931 Kentucky Medicaid 800 444 9137 For services scheduled in advance submit fax to
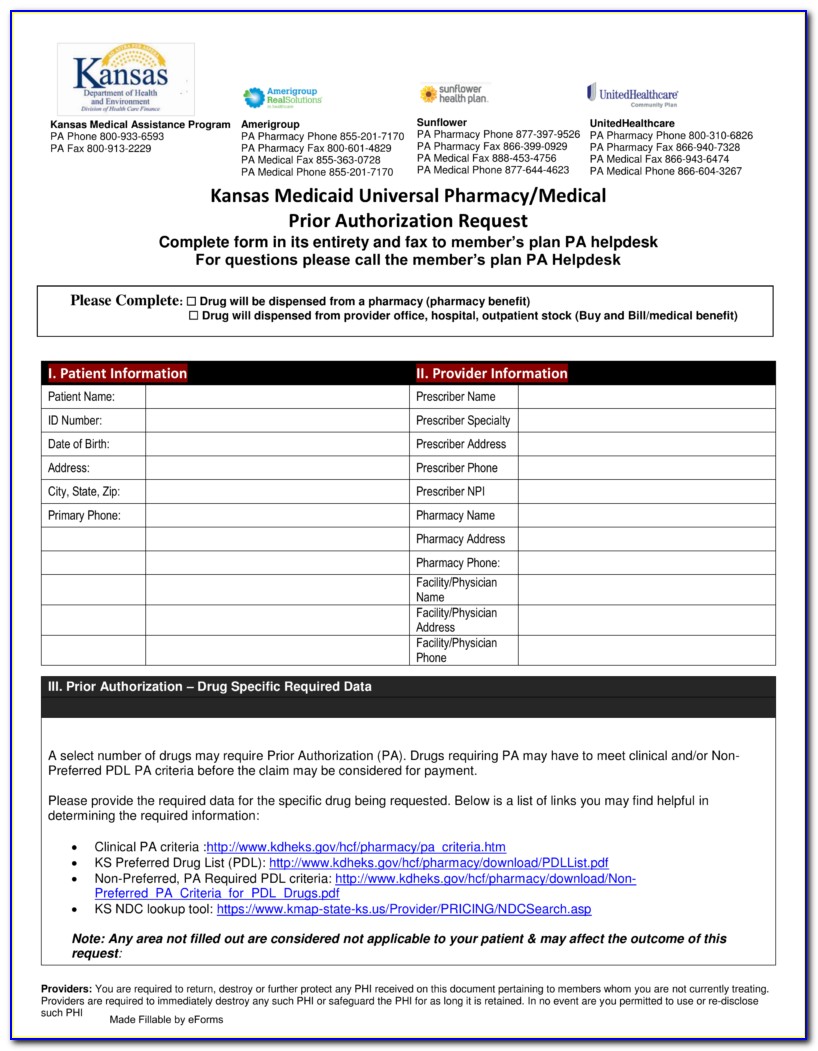
A Humana Prior Authorization Form is filled out by a pharmacist in order to help a patient secure coverage for a certain medication By submitting this form the pharmacist may be able to have the medication covered by Humana 3 Required clinical information Please provide all relevant clinical information to support a prior authorization review Please provide symptoms lab results with dates and or justification for initial or ongoing therapy or increased dose and if patient has any contraindications for the health plan insurer preferred drug
Printable Humana Prior Authorization Form
Printable Humana Prior Authorization Form
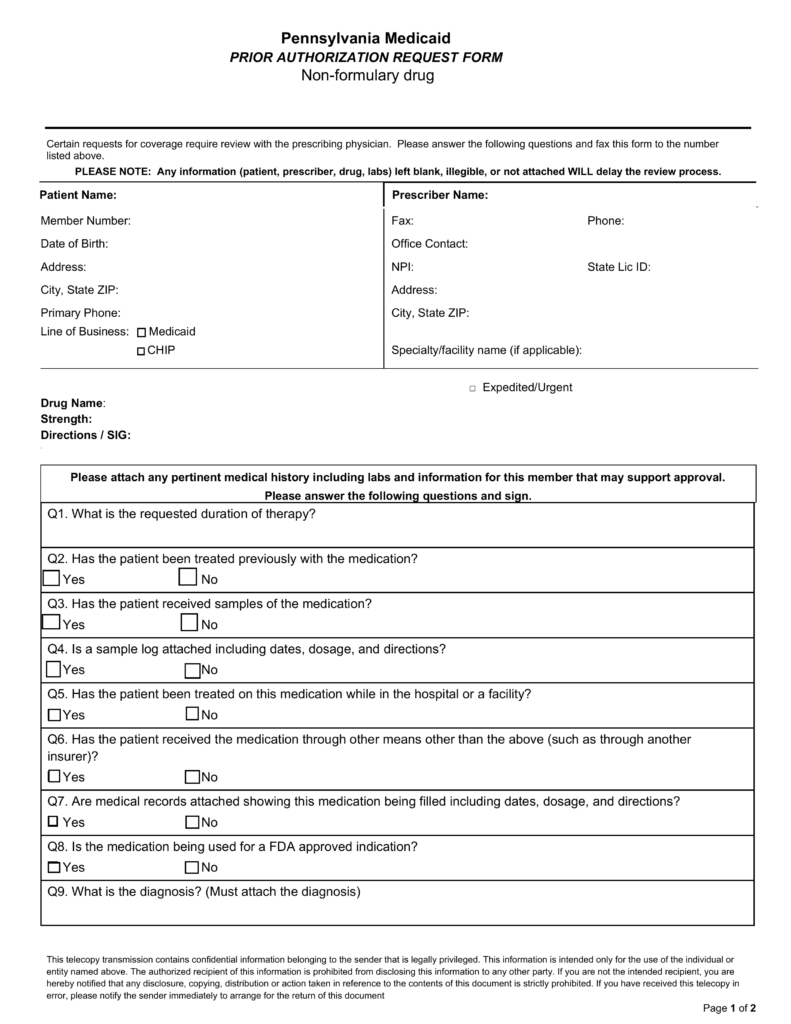
https://eforms.com/images/2017/06/Pennsylvania-Medicaid-Prior-Authorization-Form-791x1024.png
Covermymeds Humana Prior Auth Form Prior Authorization Can Help Lower The Cost Of Expensive
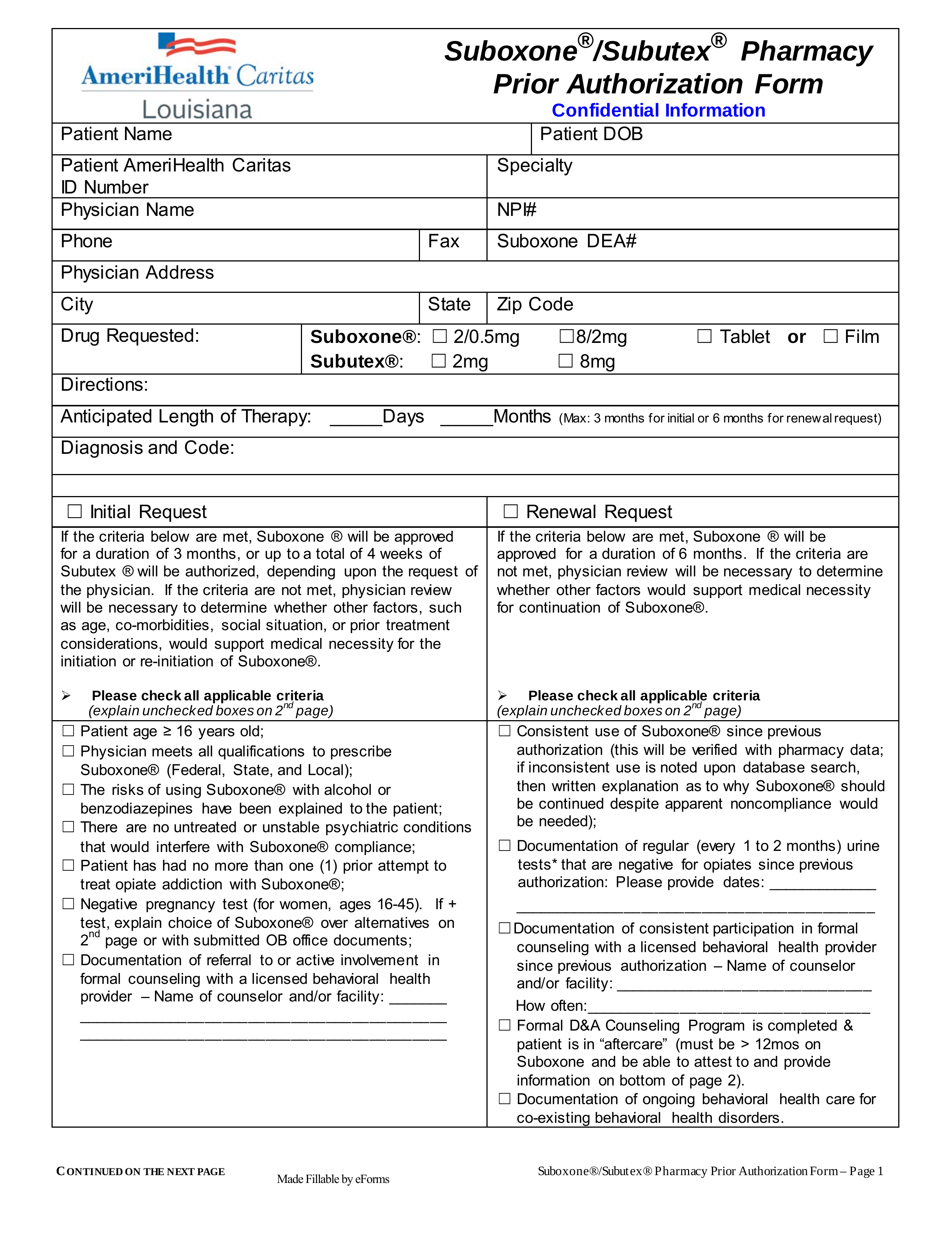
https://lh3.googleusercontent.com/proxy/kMlAYd3U6t_lbjb9HhRUAvOCIlXQYnLV6ziHBeJcRYvtUyg1oi_-lDUS3XI9_-FQxISLBtcSOZO7XJqqOH9OTrw7yf6AiU2OWqumihzPYdx6sfjfLnZ90F6epIeIT3f7QVSu=w1200-h630-p-k-no-nu

Covermymeds Humana Prior Auth Form Amerigroup Prior Authorization Form Ny Form Resume
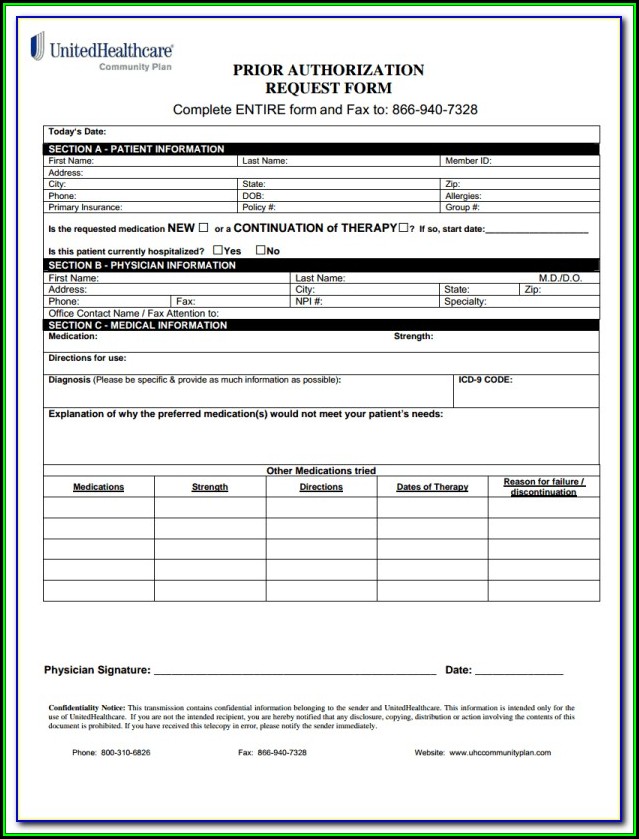
https://www.viralcovert.com/wp-content/uploads/2018/10/prior-authorization-form-for-medicare-part-a-700x869.jpg
Preauthorization tool Find answers to frequently asked questions and how to receive immediate preauthorization determinations Humana has enhanced its approval process on the Availity web portal with a new preauthorization automation feature Yes Humana sends HealthHelp an eligibility file monthly If the member is not on the eligibility file the HealthHelp representative logs onto the Humana website to check eligibility How does the authorization request process work The ordering physician s office engages HealthHelp prior to scheduling the procedure treatment to be ordered
If you have 10 or fewer drugs please select the Direct Member Reimbursement tab If you have more than 10 drugs or a compound drug please use the DMR form C for Commercial members or the DMR form M for Medicare members When you have completed the form please return to this page and select the Direct Member Reimbursement tab Amount paid TRICARE Prime TRICARE Prime requires referrals for specialist office visits and some diagnostic services if you receive services that require a referral without obtaining one you are using your Point of Service POS option Your PCM works with Humana Military for the referral and authorization
More picture related to Printable Humana Prior Authorization Form
Free Humana Prior Rx Authorization Form Pdf Eforms Vrogue
https://eforms.com/images/2017/05/AmeriHealth-Caritas-Pennsylvania-Prior-Authorization-Form.png
Covermymeds Humana Prior Auth Form Electronic Prior Authorization Solutions CoverMyMeds
https://www.contrapositionmagazine.com/wp-content/uploads/2019/01/aarp-optumrx-prior-authorization-form.jpg

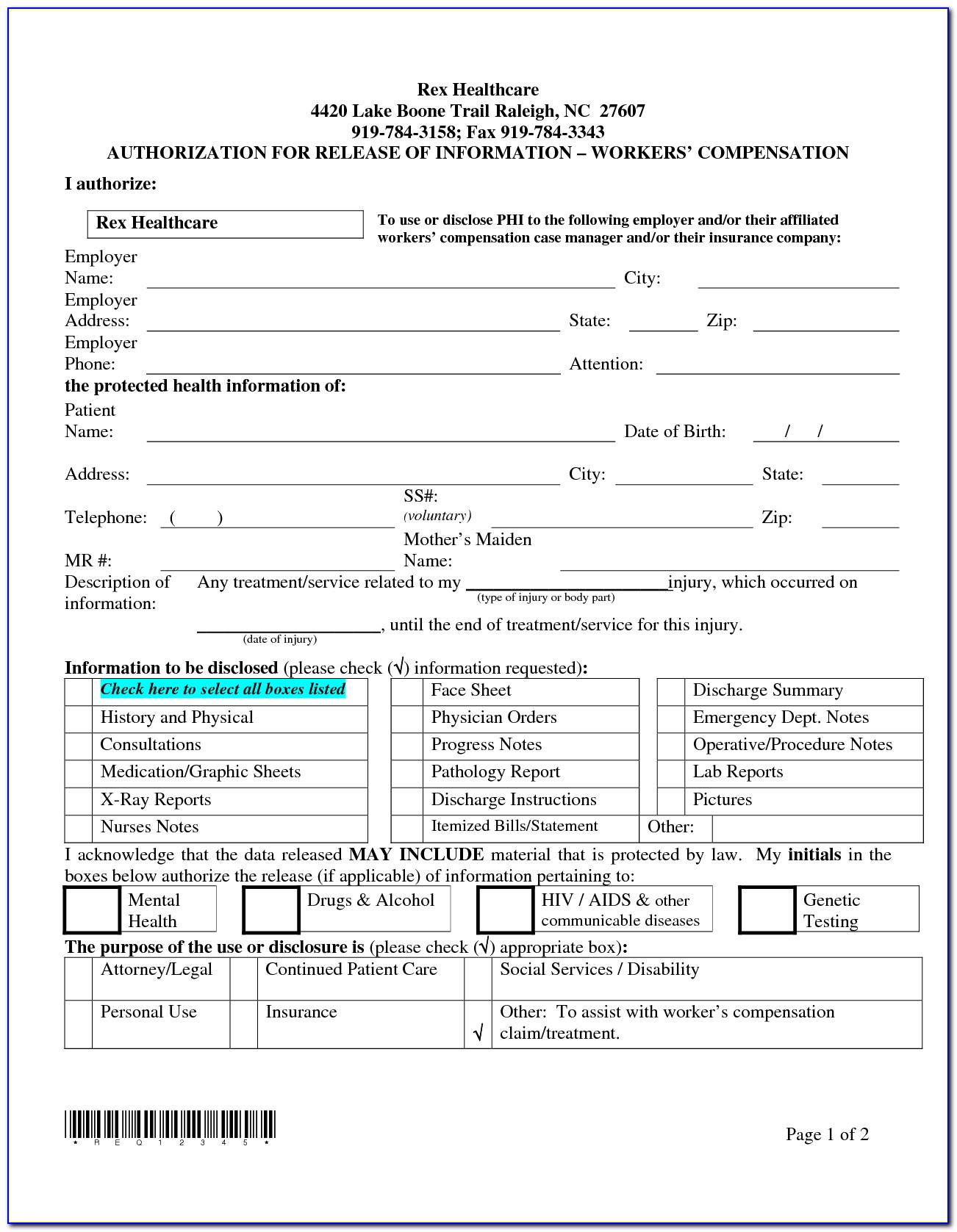
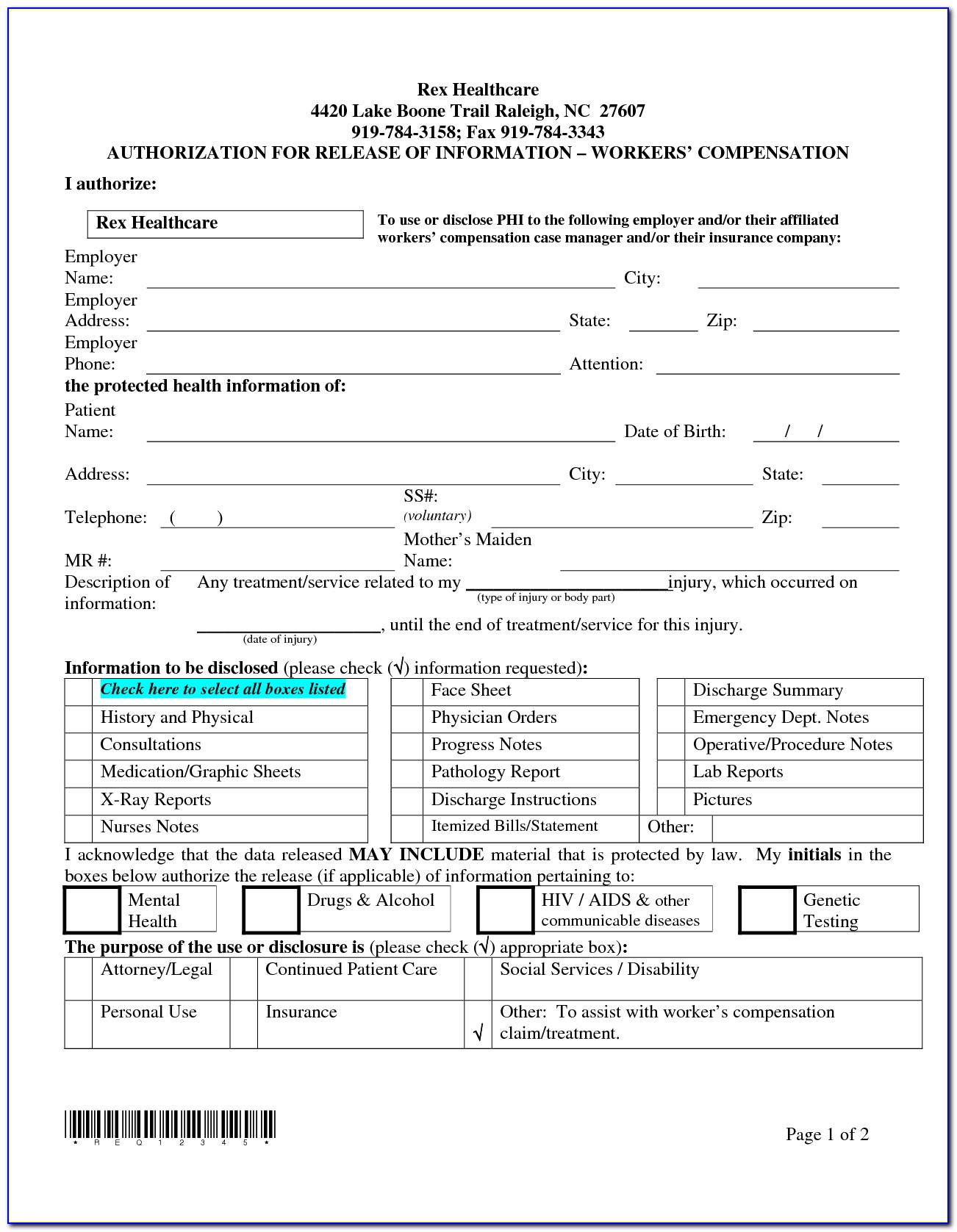
FREE 41 Authorization Forms In PDF Excel MS Word
https://images.sampleforms.com/wp-content/uploads/2017/03/Medicare-Prior-Authorization-Form.jpg
Arizona standard prior authorization request form for health care services reason v slrvxls cpt or coo o supporting v c unka title az form png author jes7499 created date Humana and Availity have teamed up to make it easy for you to work with us online The Availity Provider Portal is now Humana s preferred method for medical and behavioral health providers to check eligibility and benefits submit referrals and authorizations manage claims and complete other secure administrative tasks online
877 548 1547 Submit by phone 800 444 5445 Behavioral healthcare referrals and authorizations HumanaMilitary login Fax Outpatient Treatment Report OTR 877 378 2316 Phone 800 444 5445 Tips for making referrals and authorizations Submitting a request online at HumanaMilitary Authorization request complete Check Status box Humana has contracted with HealthHelp to review clinical requests using an evidence based approach HealthHelp s innovative and collaborative program Consult empowers physicians to request the most appropriate care for patients through peer to peer consultations for procedures
Covermymeds Humana Prior Auth Form Medco Prior Authorization Form Medicare Part D Form
https://www.viralcovert.com/wp-content/uploads/2018/10/bcbs-prior-authorization-form-florida.jpg
Humana Prior Authorization Form Fill Out And Sign Printable PDF Template SignNow
https://www.signnow.com/preview/5/585/5585489/large.png
https://docushare-web.apps.external.pioneer.humana.com/Marketing/docushare-app?file=3886584
Authorization Referral Request Form Please complete all fields on this form and be sure to include an area code along with your telephone and fax numbers To verify benefits call commercial 800 448 6262 Medicare 800 457 4708 Florida Medicaid 800 477 6931 Kentucky Medicaid 800 444 9137 For services scheduled in advance submit fax to
https://eforms.com/prior-authorization/humana/
A Humana Prior Authorization Form is filled out by a pharmacist in order to help a patient secure coverage for a certain medication By submitting this form the pharmacist may be able to have the medication covered by Humana

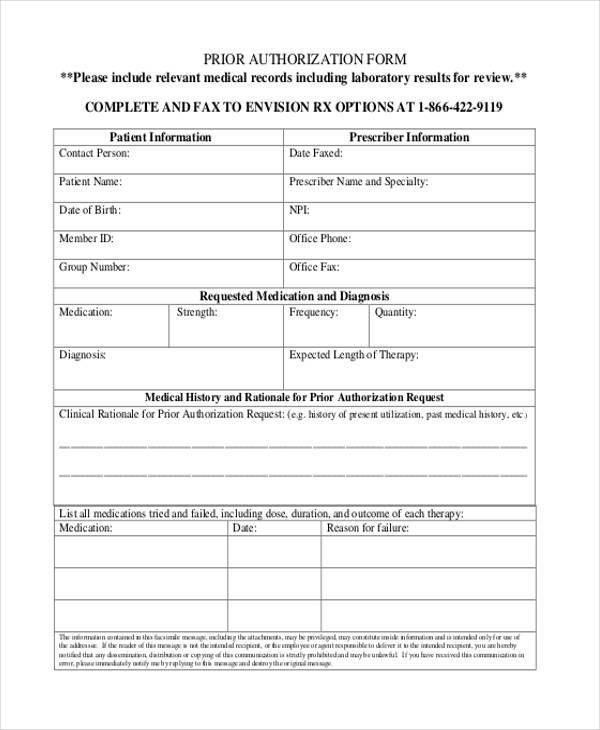
FREE 8 Sample Prior Authorization Forms In PDF MS Word
Covermymeds Humana Prior Auth Form Medco Prior Authorization Form Medicare Part D Form
Prior Authorization Letter Sample
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
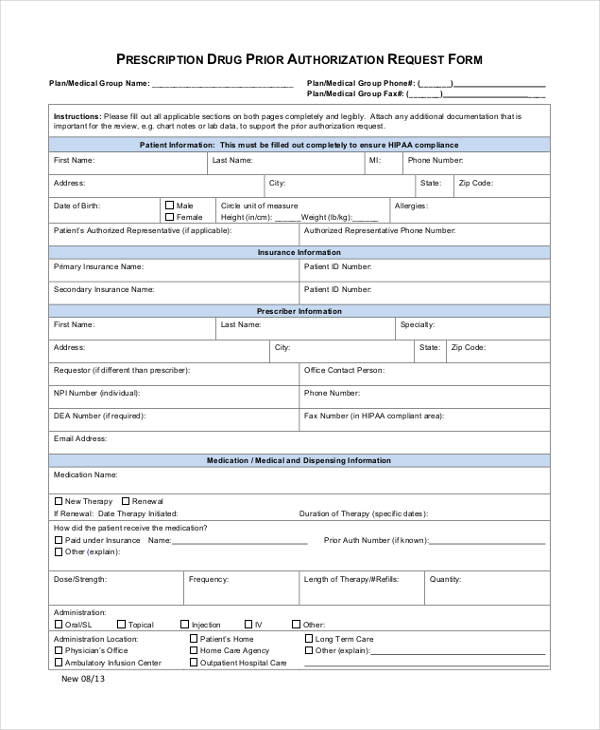
FREE 13 Prior Authorization Forms In PDF MS Word
FREE 11 Prior Authorization Forms In PDF MS Word
FREE 11 Prior Authorization Forms In PDF MS Word

Covermymeds Humana Prior Auth Form Electronic Prior Authorization Solutions CoverMyMeds

CIGNA Healthcare Prior Authorization Form 2010 2021 Fill And Sign Printable Template
Free Humana Prior Rx Authorization Form PDF EForms
Printable Humana Prior Authorization Form - We believe in equal access for all Learn more by visiting our non discrimination notice and accessibility support pages Florida residents can research healthcare information and compare drug prices pharmacies hospitals and prescribers by going to FloridaHealthFinder gov You must be 18 or older a resident of the U S and meet additional eligibility criteria to qualify